When Skin Diseases Look Alike: How Reflectance Confocal Microscopy Helps Dermatologists Avoid Misdiagnosis Without Biopsy
2026-01-09 17:18When Skin Diseases Look Alike:
How Reflectance Confocal Microscopy Helps Dermatologists Avoid Misdiagnosis Without Biopsy
In daily dermatology practice, few situations are more frustrating than this:
a patient presents with a classic-looking lesion, the clinical picture seems familiar, yet something does not fully add up. Is it psoriasis—or could it be pityriasis rosea? Is this vitiligo—or merely post-inflammatory hypopigmentation?
These diagnostic crossroads are common, even for experienced clinicians. Many inflammatory and pigmentary disorders share overlapping clinical features, especially in early or atypical stages. Traditionally, when doubt persists, a skin biopsy becomes the default solution. While histopathology remains the gold standard, it is invasive, time-consuming, and not always well accepted by patients—particularly when lesions are located on cosmetically sensitive areas.
Over the past decade, reflectance confocal microscopy (RCM) has gradually changed how dermatologists approach such diagnostic dilemmas. By allowing real-time, in vivo visualization of skin structures at near-histologic resolution, RCM offers a unique opportunity to differentiate clinically similar diseases without breaking the skin barrier.
This article walks through how RCM helps distinguish commonly confused skin conditions, starting from normal skin architecture and moving into real-world differential diagnosis—based on patterns dermatologists actually see in practice.
Why Clinical Similarity Leads to Diagnostic Errors in Dermatology
Dermatology is, by nature, a visual specialty. Pattern recognition plays a central role, but visual similarity can be deceptive.
Inflammatory erythematous plaques, scaling disorders, and hypopigmented patches often follow shared biological pathways: epidermal turnover changes, inflammatory cell infiltration, or melanocyte dysfunction. As a result, distinct diseases may appear strikingly alike on the surface, particularly when influenced by factors such as skin type, lesion location, disease stage, or prior treatment.
Several studies have shown that misdiagnosis rates are highest in:
Early-stage inflammatory dermatoses
Atypical or partially treated lesions
Hypopigmented disorders in darker skin types
RCM does not replace clinical judgment. Instead, it adds a structural dimension to clinical observation, allowing the clinician to look beneath the surface and confirm—or refute—initial impressions.
Normal Skin Architecture Under Reflectance Confocal Microscopy
Before interpreting disease patterns, it is essential to understand how normal skin appears under RCM, as all pathological changes are deviations from this baseline.
Under reflectance confocal microscopy, normal skin reveals a highly organized, layered structure:
Epidermis
Stratum corneum: Appears as bright, amorphous reflective structures without nuclei
Granular and spinous layers: Keratinocytes are polygonal with dark nuclei and bright cytoplasm, forming a regular honeycomb pattern
Basal layer: Characterized by bright rings corresponding to melanin-rich basal keratinocytes surrounding dark dermal papillae
Dermo-epidermal junction (DEJ)
Well-defined papillary rings
Uniform architecture with evenly spaced dermal papillae
Superficial dermis
Fine collagen fibers
Occasional small blood vessels with normal caliber
This organized appearance serves as a reference point. Any disruption—loss of pigment rings, architectural disarray, inflammatory cell clusters, or vascular distortion—immediately signals pathology.
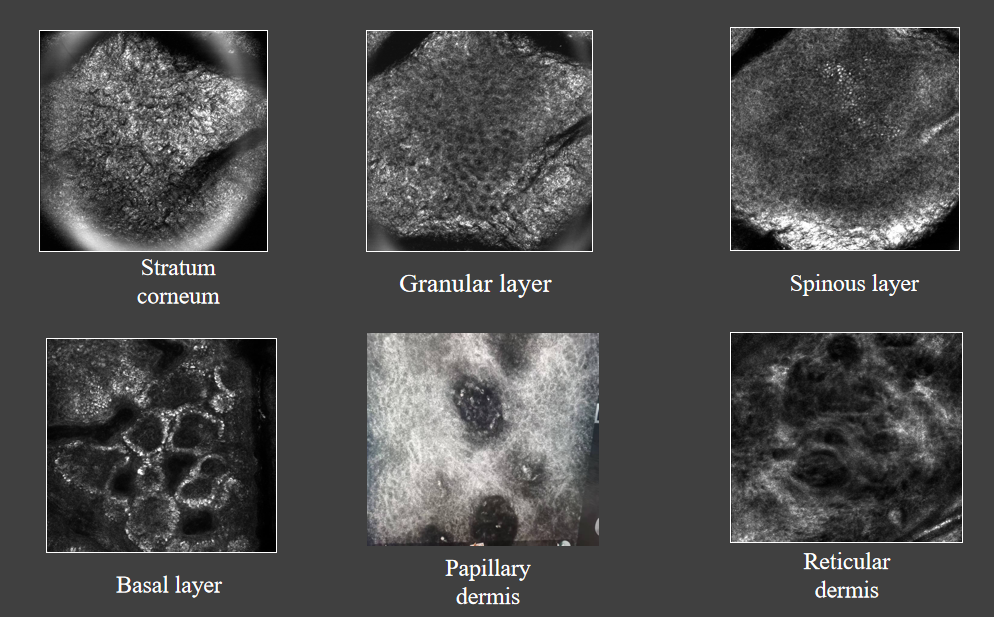
Figure 1. Normal Skin Architecture Under Reflectance Confocal Microscopy (RCM)
Reflectance confocal microscopy of normal skin demonstrates a well-organized epidermal structure. The stratum corneum appears as bright, anucleated reflective material. The spinous layer shows a regular honeycomb pattern of keratinocytes. At the dermo-epidermal junction, intact and evenly distributed pigment rings surround dermal papillae, indicating normal melanocyte distribution and epidermal architecture.
RCM in Differentiating Commonly Confused Skin Diseases
Psoriasis vs Pityriasis Rosea
A classic diagnostic challenge

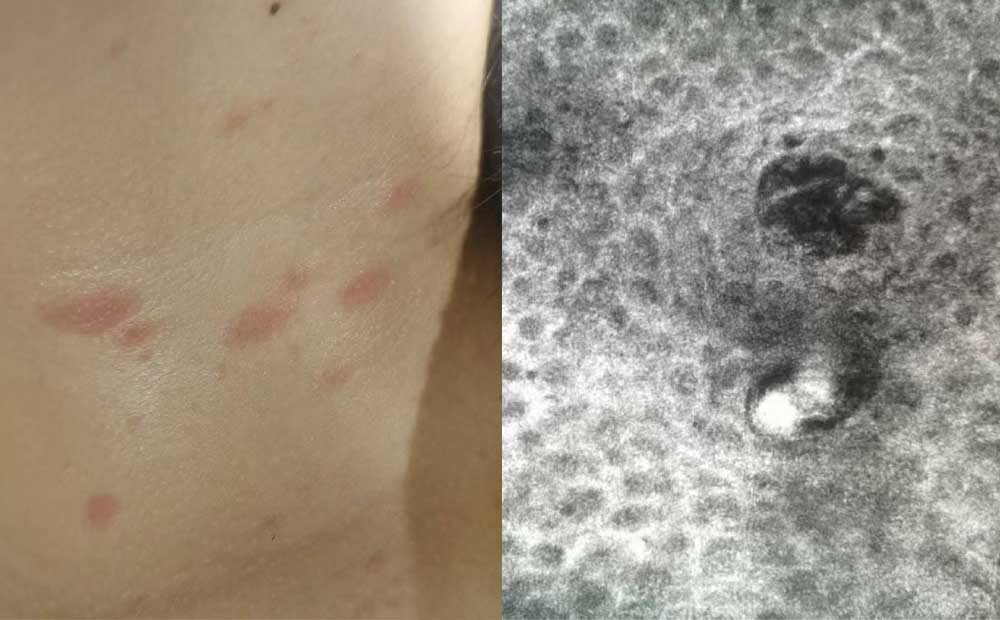
Figure 2. Psoriasis: Characteristic RCM Features
RCM imaging of psoriatic lesions reveals pronounced parakeratosis with clusters of nucleated cells in the stratum corneum, corresponding to Munro microabscesses. The normal honeycomb pattern of the epidermis is disrupted. Marked dilation and tortuosity of dermal papillary vessels are observed, reflecting the hyperproliferative and inflammatory nature of psoriasis.
Clinically, both psoriasis and pityriasis rosea may present as erythematous, scaly plaques. In early or atypical cases, differentiation based solely on morphology can be difficult.
Psoriasis
Clinical background:
Psoriasis typically presents as well-demarcated erythematous plaques covered with silvery-white scale. Auspitz sign and the presence of thickened plaques are helpful clues, but not always evident.
RCM features:
Under RCM, psoriasis demonstrates several characteristic findings:
Parakeratosis combined with hyperkeratosis
Clusters of nucleated cells in the stratum corneum, corresponding to Munro microabscesses
Marked elongation and dilation of dermal papillary vessels, often appearing tortuous
Loss of normal honeycomb pattern due to accelerated keratinocyte turnover
These features reflect the hyperproliferative and inflammatory nature of psoriasis at a microscopic level.
(Suggested image placement: RCM image showing Munro microabscesses and dilated papillary vessels)
Figure 3. Pityriasis Rosea: Subtle Inflammatory Changes on RCM
In pityriasis rosea, RCM shows focal and mild parakeratosis with preservation of overall epidermal architecture. Mild spongiosis is present within the spinous layer, consistent with intercellular edema. Superficial dermal vessels appear slightly dilated but lack the pronounced tortuosity seen in psoriasis.
Pityriasis Rosea
Clinical background:
Pityriasis rosea is generally self-limited, often following a herald patch and characterized by oval lesions aligned along skin cleavage lines. Viral triggers have been proposed, though the exact etiology remains unclear.
RCM features:
RCM findings are subtler compared with psoriasis:
Focal and mild parakeratosis
Mild spongiosis within the spinous layer, reflecting intercellular edema
Slight dilation of superficial dermal vessels, without marked tortuosity
Preservation of overall epidermal architecture
These differences, while subtle, are often sufficient to distinguish pityriasis rosea from psoriasis without resorting to biopsy.
Vitiligo vs Nevus Depigmentosus vs Post-inflammatory Hypopigmentation
Hypopigmented lesions are another frequent source of diagnostic uncertainty, especially in children and young adults.

Figure 4. Vitiligo: Loss of Pigment Rings on RCM
RCM examination of vitiligo lesions demonstrates a marked reduction or complete absence of basal layer pigment granules. Pigment rings at the dermo-epidermal junction are partially or completely absent, indicating melanocyte loss or severe dysfunction. The transition between lesional and non-lesional skin is sharply demarcated.
Vitiligo
Pathophysiological background:
Vitiligo is an acquired depigmenting disorder driven by autoimmune destruction or dysfunction of melanocytes in genetically predisposed individuals.
RCM features:
Marked reduction or complete absence of basal layer pigment granules
Loss or disruption of pigment rings at the dermo-epidermal junction
Sharply demarcated transition between affected and unaffected skin
These findings correlate directly with melanocyte loss and are highly characteristic.
(Suggested image placement: RCM image showing absent pigment rings)

Figure 5. Nevus Depigmentosus: Preserved Pigment Rings Despite Hypopigmentation
In nevus depigmentosus, RCM reveals mildly reduced basal pigmentation while maintaining intact pigment rings at the dermo-epidermal junction. Epidermal architecture remains preserved, supporting the diagnosis of a stable, non-progressive congenital hypopigmented lesion.
Nevus Depigmentosus
Clinical background:
Nevus depigmentosus is a congenital, non-progressive hypopigmented lesion, usually stable throughout life.
RCM features:
Slightly reduced basal pigmentation
Intact pigment rings
Preserved epidermal architecture
The key distinction from vitiligo lies in the preservation of pigment rings and structural stability.

Figure 6. Post-inflammatory Hypopigmentation: Residual Inflammatory Signatures
RCM findings in post-inflammatory hypopigmentation include slight reduction of basal pigmentation with preservation of pigment rings. Scattered melanophages are visible in the superficial dermis, reflecting prior inflammatory activity rather than permanent melanocyte destruction.
Post-inflammatory Hypopigmentation
Clinical background:
This condition follows inflammatory dermatoses or trauma, where melanocyte function is temporarily impaired rather than destroyed.
RCM features:
Mild reduction in basal pigmentation
Presence of pigment-laden macrophages in the superficial dermis
Preserved pigment ring structure
This combination helps clinicians avoid overdiagnosing vitiligo in reversible conditions.
Why Reflectance Confocal Microscopy Matters in Clinical Practice

Figure 7. Comparative Overview: RCM Patterns in Clinically Similar Skin Disorders
Side-by-side RCM images highlight the diagnostic value of confocal imaging in differentiating clinically similar skin conditions. Distinct differences in pigment distribution, epidermal architecture, inflammatory cell presence, and vascular patterns allow accurate, noninvasive diagnosis without the need for immediate biopsy.
From a clinician’s perspective, the value of RCM lies not only in diagnostic accuracy, but also in clinical confidence and patient communication.
RCM allows dermatologists to:
Reduce unnecessary biopsies
Monitor disease progression and treatment response
Provide visual explanations to patients
Improve diagnostic precision in cosmetically sensitive areas
As dermatology continues to move toward precision and patient-centered care, RCM has become an increasingly indispensable tool—bridging the gap between clinical observation and histopathology.
From Pattern Recognition to Structural Confirmation:
Why RCM Is Becoming Clinically Indispensable
What these examples have in common is not complexity, but similarity. Psoriasis and pityriasis rosea may look alike on the surface. Vitiligo, nevus depigmentosus, and post-inflammatory hypopigmentation may all present as pale patches to the naked eye. Yet beneath the epidermis, their biological behavior is fundamentally different.
Reflectance confocal microscopy allows dermatologists to move beyond descriptive morphology and into structural confirmation. By visualizing epidermal architecture, pigment distribution, inflammatory patterns, and vascular changes in vivo, RCM helps clinicians answer a critical question at the bedside: Are we seeing the same disease—or merely similar-looking ones?
In many cases, this additional layer of information is enough to:
Avoid invasive biopsy procedures
Prevent delayed or inappropriate treatment
Reduce patient anxiety caused by diagnostic uncertainty
Support earlier, more targeted therapeutic decisions
Importantly, RCM does not replace histopathology. Instead, it acts as a bridge between clinical observation and biopsy, narrowing diagnostic possibilities and reserving invasive procedures for cases where they are truly necessary.
Clinical Confidence Matters—For Doctors and Patients Alike
From a practical standpoint, one of the most underappreciated benefits of RCM is its impact on clinical confidence. When clinicians can correlate what they see clinically with what they observe microscopically—without waiting days for pathology reports—decision-making becomes more assured and transparent.
Patients, too, benefit from this immediacy. Being able to see their skin condition explained in real time fosters trust, improves adherence to treatment plans, and enhances overall satisfaction with care. This is particularly meaningful in chronic or cosmetically sensitive conditions, where repeated biopsies are neither ideal nor well tolerated.
The Role of RCM in Modern Dermatology Practice
As dermatology evolves toward more precise, patient-centered care, tools that offer noninvasive, high-resolution, repeatable imaging are no longer optional. They are becoming part of the standard diagnostic workflow in advanced dermatology centers worldwide.
RCM is especially valuable in:
Inflammatory dermatoses with overlapping clinical features
Pigmentary disorders requiring longitudinal monitoring
Lesions located on the face or other sensitive areas
Situations where biopsy is contraindicated or undesirable
Its growing adoption reflects a broader shift in dermatology: from relying solely on visual pattern recognition to integrating real-time microstructural evidence into everyday practice.
Looking Ahead: Practical Technology Serving Real Clinical Needs
Behind every effective diagnostic tool lies thoughtful engineering guided by clinical reality. Modern RCM systems are increasingly designed with daily dermatology workflows in mind—prioritizing image stability, ease of operation, and consistent image quality across different skin types and lesion locations.
For clinicians seeking to integrate confocal imaging into routine practice, the focus is no longer on novelty, but on reliability, reproducibility, and clinical relevance. Equipment must support—not complicate—clinical decision-making.
KernelMed’s work in reflectance confocal microscopy follows this same philosophy: translating advanced optical imaging principles into practical systems that align with real-world dermatology needs. By emphasizing image clarity, operational stability, and clinical usability, such systems aim to make confocal imaging accessible not only in academic centers, but also in high-volume clinical settings.
More information on KernelMed’s dermatology imaging solutions can be found at:
👉 RCM System
Final Thoughts
In dermatology, what looks similar is not always the same—and the difference matters. Reflectance confocal microscopy offers a powerful, noninvasive way to uncover those differences, helping clinicians see beyond the surface and practice with greater precision.
As clinical demands continue to rise and patient expectations evolve, tools that enhance diagnostic accuracy while preserving patient comfort will play an increasingly central role. RCM stands as one of those tools—quietly reshaping how dermatologists diagnose, differentiate, and decide.