When the Data Raises Questions: An Internal MED Verification of KernelMed’s LED 308 nm Phototherapy System
2026-01-28 17:29When “Mild Erythema” Raises a Serious Question
In ultraviolet phototherapy, erythema has long been regarded as a visible indicator of biological response. For clinicians, it often provides reassurance that ultraviolet energy has reached the target tissue. For patients, redness is sometimes interpreted as tangible proof that a treatment is “working.”
However, clinical reality is rarely that simple.
In October 2025, KernelMed received feedback from an overseas clinical partner in Iraq reporting that, during LED-based 308 nm UV phototherapy, the erythema response observed in minimal erythema dose (MED) testing appeared milder than expected. The question raised was clinically reasonable: Does a subtle erythema suggest insufficient dose delivery, or is it part of normal response variability?
Rather than offering theoretical explanations alone, KernelMed chose to verify this observation through a structured, real-world process. An internal volunteer-based MED verification was initiated, designed to reflect routine clinical testing rather than idealized laboratory conditions.
This article documents the background, methodology, and clinical insights derived from that internal verification. More importantly, it explores why erythema intensity should not be interpreted in isolation—and how evidence-based verification can improve clinical understanding, patient communication, and professional trust.
Volunteer Characteristics (Anonymized)
| Volunteer ID | Sex | Skin Reaction Pattern | MED Response Timing | Notes |
|---|---|---|---|---|
| Volunteer A | M/F | Mild erythema | Delayed | No discomfort |
| Volunteer B | M/F | Clear erythema | Typical | Within expected range |
| Volunteer C | M/F | Mild erythema | Delayed | Rapid resolution |
| Volunteer D | M/F | Moderate erythema | Typical | No adverse events |
| Volunteer E | M/F | Mild erythema | Delayed | Required observation |
| Volunteer F | M/F | Clear erythema | Typical | Stable reaction |
| Volunteer G | M/F | Very mild erythema | Late onset | High tolerance |
| Volunteer H | M/F | Moderate erythema | Typical | Self-limited |
[Figure 1. Internal MED verification setup using LED 308 nm UV phototherapy system]
Understanding MED: A Practical Tool, Not an Absolute Threshold
The minimal erythema dose (MED) is defined as the lowest ultraviolet dose that produces perceptible erythema within a standardized observation period, typically 24 hours. In dermatology, MED has traditionally served as a reference point for initiating phototherapy and ensuring treatment safety.
However, MED is often misunderstood as a fixed or universal value. In reality, it is a response-based parameter, influenced by multiple biological and technical factors, including:
Skin phototype and baseline pigmentation
Anatomical site and local vascular characteristics
Prior ultraviolet exposure and seasonal variation
Individual inflammatory sensitivity
Light source characteristics and energy delivery profile
As a result, identical ultraviolet doses may produce noticeably different erythema responses across individuals, without implying differences in therapeutic effectiveness or device performance.
Recognizing MED as a guiding framework rather than a definitive threshold is essential, particularly when evaluating newer phototherapy technologies.

[Figure 2. Inter-individual variability in minimal erythema dose (MED) response]
LED-Based 308 nm Phototherapy and Erythema Expression
Although LED-based and excimer-based systems share the same therapeutic wavelength (308 nm), their modes of energy delivery differ in clinically relevant ways.
Excimer systems typically deliver highly concentrated, monochromatic beams with sharp focal intensity, often producing rapid and visually prominent erythema. In contrast, LED-based 308 nm phototherapy systems deliver energy in a more uniform and distributed manner, resulting in broader tissue exposure with reduced focal peaks.
This difference in energy distribution may lead to:
More homogeneous epidermal exposure
Reduced localized thermal stress
A more gradual inflammatory cascade
Consequently, erythema observed during LED-based phototherapy may appear milder, even when cumulative energy delivery is clinically sufficient. Importantly, biological effects such as immunomodulation and melanocyte activation do not require intense visible erythema to occur.
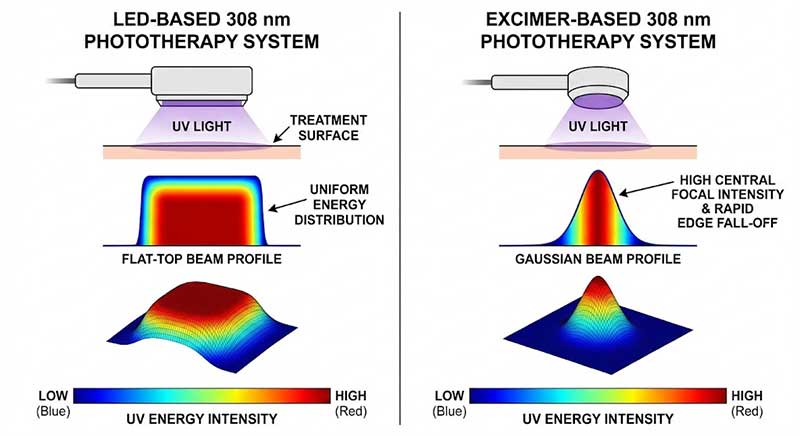
[Figure 3. Energy delivery characteristics of LED-based versus excimer-based 308 nm phototherapy]
Background: Overseas Clinical Feedback and the Decision to Verify
The feedback from Iraq reflected a real-world challenge in global clinical practice: expectations shaped by prior experience with different technologies. When erythema intensity did not align with those expectations, it naturally prompted questions.
KernelMed approached this feedback as a signal for clarification rather than confrontation. Instead of attributing the observation solely to individual variability, the company initiated an internal MED verification process to better understand erythema response patterns under controlled, reproducible conditions.
Participation was voluntary and anonymized. The purpose was not to demonstrate superiority, but to generate transparent, internally validated data that could inform clinical dialogue and education.
Study Design: Internal Volunteer-Based MED Verification
The internal verification involved healthy adult volunteers, anonymized and identified using alphabetical labels (Volunteer A–H). The study design mirrored standard clinical MED testing practices.
Key elements included:
Device: LED-based 308 nm UV phototherapy system
Exposure site: Standardized anatomical regions with consistent geometry
Dose escalation: Incremental ultraviolet exposure following established MED protocols
Observation period: Erythema assessed at 24 hours post-exposure
Evaluation criteria: Presence, intensity, and distribution of erythema
No therapeutic endpoints were evaluated. The sole objective was to observe erythema response behavior under real-world conditions.
Results: Variability Is the Rule, Not the Exception
The verification results confirmed a central principle of phototherapy: erythema response is inherently variable.
Among the volunteers, erythema onset occurred at different cumulative doses, and intensity varied despite identical exposure protocols. Some participants exhibited perceptible erythema at lower doses, while others required higher cumulative exposure for similar visual response.
Common observations included:
Diffuse erythema distribution rather than sharply demarcated redness
Non-linear relationship between dose escalation and erythema intensity
Prompt recovery without prolonged irritation
These findings reinforced that mild erythema should not be interpreted as treatment inadequacy, particularly in LED-based phototherapy systems designed for controlled energy delivery.
[Figure 4. Summary of erythema response variability among internal volunteers]
Clinical Interpretation: When Mild Erythema Is Still Meaningful
In daily practice, clinicians often rely on visual cues to guide decision-making. However, erythema intensity alone does not fully capture photobiological activity.
Therapeutic ultraviolet effects—including immunomodulation, cytokine signaling shifts, and melanocyte stimulation—occur at energy levels that may not provoke pronounced inflammation. Excessive erythema, by contrast, may represent unnecessary tissue stress rather than enhanced efficacy.
Understanding this distinction allows clinicians to:
Maintain confidence in treatment protocols
Avoid unnecessary dose escalation
Communicate more effectively with patients
LED-based 308 nm phototherapy, by design, prioritizes controlled exposure and safety, which may manifest as subtler erythema without compromising biological impact.
What This Means for Patients
For patients, visible redness is often equated with treatment success. When erythema is mild or delayed, uncertainty may arise.
Clear education is therefore critical. Patients should understand that:
Therapeutic effects are cumulative and not immediately visible
Redness intensity does not predict long-term outcomes
Consistency and safety outweigh aggressive dosing
Reframing erythema as one of several response indicators helps reduce anxiety and supports adherence to prescribed treatment plans.
[Figure 5. Typical erythema onset and resolution following LED-based 308 nm UV exposure]
Implications for Clinical Practice and Device Evaluation
From both clinical and market perspectives, this internal verification highlights the importance of contextual evaluation. Device performance should be assessed based on biological response, safety profile, and consistency—not solely on visual erythema intensity.
KernelMed’s response to overseas feedback illustrates a commitment to evidence-based clarification. By generating internal data and openly discussing variability, the company supports informed clinical decision-making and strengthens professional trust.
Conclusion: From Feedback to Evidence
The October 2025 internal MED verification was not intended to redefine phototherapy standards, but to better understand real-world response patterns. By responding to clinical feedback with structured observation rather than assumption, KernelMed reaffirmed a fundamental principle of medical practice: evidence guides interpretation.
Mild erythema observed during LED-based 308 nm UV phototherapy does not indicate reduced effectiveness. Instead, it reflects the complex interaction between technology, biology, and individual variability—an interaction best understood through transparent verification and clinical dialogue.